Dry eyes / office eye syndrome
One in five patients who consult an ophthalmologist in Germany suffers from dry eyes—a disorder of the natural tear film. These symptoms manifest themselves as burning, itching, or tearing.
These symptoms are collectively referred to as office eye syndrome, as they occur particularly when we are sitting at a computer or otherwise concentrating and forget to blink.
However, various diseases such as diabetes, rheumatism, or thyroid dysfunction can also cause insufficient tear production.
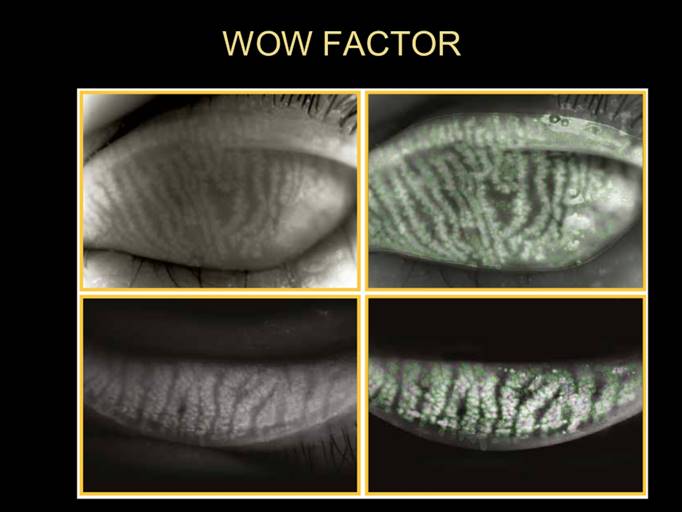
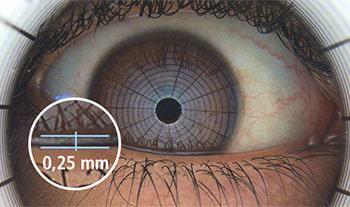
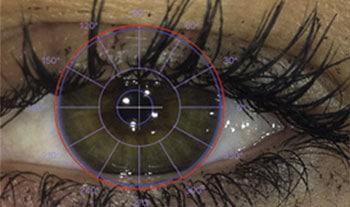
In our practice, we use various tests to determine the extent of the tear film disorder. The Schirmer test is important here: small strips of absorbent paper are placed in the conjunctival sac to measure the time it takes for them to become saturated. By applying a dye to the surface of the eye and asking you not to blink, we can determine how stable the tear film is.
In addition to special eye drops, small changes in everyday behavior can often help, e.g., taking breaks when working at a computer screen, drinking enough fluids, or improving the supply of fresh air.
Dry eyes should be taken seriously, because what may seem like a minor annoyance at first can lead to disease of the eye surface and thus to a loss of vision.